Achieving Regulatory Compliance

Author: Maxwell Healthcare Associates Posted: September 1, 2020
What does compliance really mean in the home health industry? Agencies who look to be compliant aim to eliminate fraud, abuse, and waste within their organizations. Beyond the obvious avoidance of fraud and abuse, an investment into a sound compliance program for agencies of all sizes is advisable.
A day in the life of a home health provider
Let’s get into what life looks like for a home health provider as we set the stage for compliance within the industry.
- Clinicians are sent out into the field to provide services primarily to the elderly population across the nation. Unfortunately, our clientele is clearly at a high risk for fraud and abuse.
- We live by and accept terms of an agreement that are set forth in a contract with the federal government and depend on those same clinicians and back office personnel to uphold those standards (i.e. CMS/Medicare).
- Under the terms of that very agreement with CMS, we accept monetary payments for the care that we provide based on an assessment that our clinicians complete (Our OASIS assessment determines how much we get paid). We are the only sub-section of the HHS that does this.
- Not only do we decide how much we get paid, we decide if it is appropriate or not to get paid. For example, we tend to ask the following questions to determine payment:
- Is the patient homebound,
- Do they meet criteria?
- Do they have a skilled need?
For the most part in terms of a provider or organization we are depending once again on someone else to do this. For many organizations of any size, we allow our clinicians (nurses, therapists, and sometimes aides) and back office personnel to truly decide our fate. While a certification must come from the physician, it is our responsibility to decide whether we have the right documentation to support that certification. We also have the responsibility of carrying out all of the items mentioned above.
OIG enforcements
According to the Home Health Compliance with Medicare Requirement’s Workplan based on a 2014 determination by CMS’s Comprehensive Error Rate Testing (CERT) program, 51.4 percent or about 9.4 billion in home health payments were inaccurate. The inaccurate findings are primarily related to two things: homebound status and need for skilled services.
In these eight OIG specific audits, a total of 420,849 dollars in overpayment with a total calculated estimate of overpayments added up to just over 37 million dollars. The breakdown of each of these audits is diagrammed below:
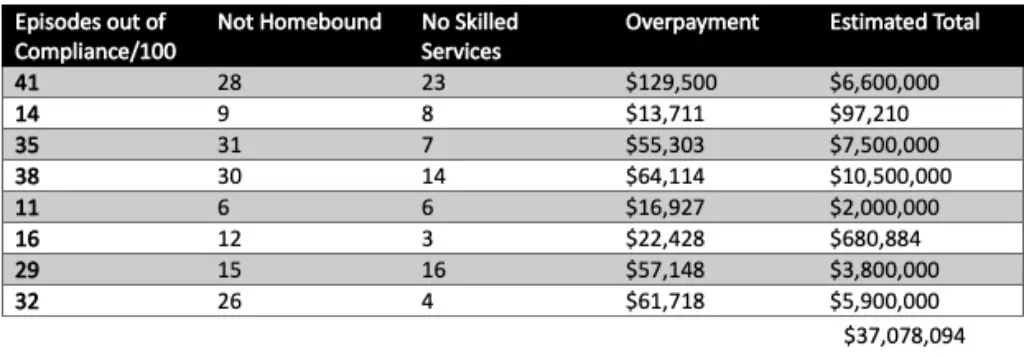
These are some pretty scary numbers and these audits are not going stop.
Why are you getting denied?
- Homebound Status – We have very specific guidelines that can and should always be followed. Why are organizations getting denied?
- No Skilled Services – We also have very clear and specific guidelines as to what constitutes a skilled need, the same questions arrive in my mind.
Organizations know the regulations and have policies and procedures that guide us through validating these very things (homebound status and skilled need). However, organizations must ask the following questions to delve deeper into the topic:
- Do we ensure that these policies are followed?
- Do we give realistic thought and consideration to our regulatory review process?
- Do we truly follow our compliance plan that is required by CMS?
At MHA, we see examples of great policies and procedures and well written regulatory compliance plans, but true compliance and follow through are not so common. Also, we often see organizations that have in some ways outgrown themselves, and they at times have some contradicting processes across different regions/sub-sections of their organization.
Staying compliant and avoiding denials
- Train employees to understand policies and procedures related to eligibility, certification, and homebound status.
- Keep employees up to date with any changes and or updates to CMS regulations and/or policy and procedure changes.
- Create a comprehensive compliance plan that includes a process to reconcile any issues identified.
- Ensure that there is a clear path of responsibility and a process for holding violators accountable.
- Review and update your compliance plan frequently to ensure that your plan is always up to date.
Regulatory compliance is a complex topic to navigate. Without proper guidance or instruction, many organizations will likely make avoidable mistakes. Thankfully, you have Maxwell Healthcare Associates who can assist with your compliance and regulatory needs. MHA has a robust operations team with several years of compliance experience to assist you with compliance issues. Contact us today to learn how MHA can help your organization remain compliant.
