Embrace the OASIS-E (Part 3)

Author: Leigh Massey, RN, JD, WOCN, CHC, CHPC
Posted: September 13, 2022
CMS introduced OASIS-E changes for Home Health Agencies to meet the requirements of the IMPACT Act and improve interoperability among the post-acute continuum. The Act requires implementation of standardized quality measures and the development and reporting of measures pertaining to resource use, hospitalization, and discharge to the community. These requirements are reflected in the OASIS – E tool as new assessments:
- Reconciled Medication List (Section A)
- Cognitive Patterns (Section C)
- Signs and Symptoms of Delirium from CAM (Section C)
- Mood – Expand PHQ-2 to PHQ09 (Section D)
This article will address the changes to the OASIS related to Cognitive Patterns, Signs and Symptom of Delirium and Mood. (See part 2 for assessments related to the Medication List reconciliation.)
Cognitive Patterns (Section C)
Cognitive Patterns and signs and symptoms of Delirium are housed in Section C on the OASIS – E tool. These items were addressed in earlier versions of the OASIS; however, this version expands and standardizes the assessments to get a better understanding of a patient’s base line status. This might support clinical decision making, care coordination, cost reduction, and improved patient and family experiences. Like the other assessments, this will be completed across all post-acute care (PAC) settings.
Cognitive Patterns and signs and symptoms of Delirium are housed in Section C on the OASIS – E tool. These items were addressed in earlier versions of the OASIS; however, this version expands and standardizes the assessments to get a better understanding of a patient’s base line status. This might support clinical decision making, care coordination, cost reduction, and improved patient and family experiences. Like the other assessments, this will be completed across all post-acute care (PAC) settings.
Changed items from OASIS – D1 to OASIS – E
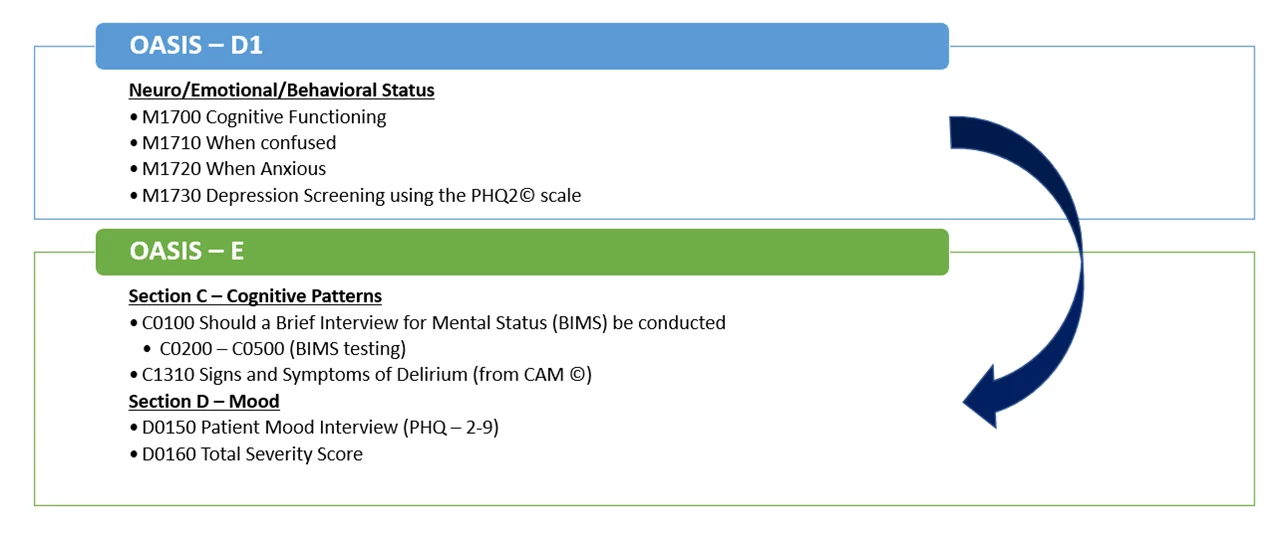
Items in OASIS – D1 are being eliminated or updated for the OASIS – E version. This is a key change for assessing clinicians and coders. This needs attention and intense training on how these assessments will be conducted and scored.
One new assessment is the BIMS, an acronym for Brief Interview for Mental Status. It is a performance based cognitive assessment. BIMS is not meant to diagnose a cognitive disorder but can provide baseline information about cognitive function and help with the development of care plans and achieve quality outcomes. It is also important to assess because cognitive functioning is a determining factor in how patients can self-manage their disease state and is linked to rehospitalization rates.
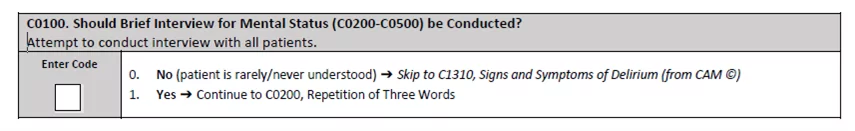
C0100. Should Brief Interview for Mental Status be Conducted?
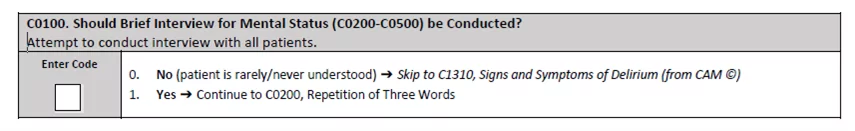
This item is used to determine whether the BIMS, a structured cognitive interview should be conducted on Start of Care (SOC), Resumption of Care (ROC) or Discharge from agency (DC). Without an attempted structured cognitive interview, some patients may appear more cognitively intact than they are. This test provides insight into the patient’s current condition that will enhance good care.
To ensure the assessments are conducted consistently each time, the OASIS – E Guidance Manual provides general guidance for C0200 – C0500, including basic BIMS interview instruction and cue cards for administering the BIMS in written format, as well as specific guidance on the individual items.
C0200-C0500: Brief Interview for Mental Status (BIMS)
This section is composed of a series of question assessments
C0200: Repetition of Three Words
C0300: Temporal Orientation (Orientation to year, month, and day) C0400: Recall (of the words from item C0200)
C0500: BIMS Summary Score
The intent of this item is to determine the patient’s attention, orientation, and ability to register and recall information.
- Direct or performance-based testing of cognitive function decreases the chance of incorrect labeling of cognitive ability and improves detection of delirium.
- Cognitively intact patients may appear to be cognitively impaired because of a language barrier, hearing impairment, or lack of social interaction.
- Some patients may appear to be more cognitively intact than they are.
- If cognitive impairment is incorrectly diagnosed or missed, appropriate communication, worthwhile activities and therapies may not be offered.
C1310: Signs and Symptoms of Delirium
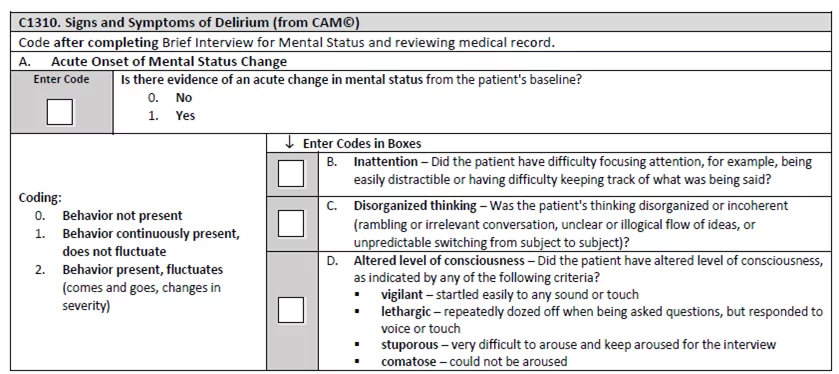
The intent of this item is to identify any signs or symptoms of acute mental status changes as compared to the patient’s baseline status and will be assessed at SOC, ROC and DC.
Delirium is defined by CMS as a mental disturbance characterized by new or acutely worsening confusion, disordered expression of thoughts, change in level of consciousness or hallucinations. It can be misdiagnosed as dementia but may be reversible if acute and addressed timely.
Delirium is associated with
- Increased Mortality
- Functional Decline
- Development or Worsening of Incontinence, Behavior Problems,
- Withdrawal from Activities
- Rehospitalizations and Increased Length of Home Health Stay
These reasons make it clear that this assessment will help predict goals, interventions, and outcomes for the home health episode.
Section D – Mood
D0150. Patient Mood Interview (PHQ -2 to 9)
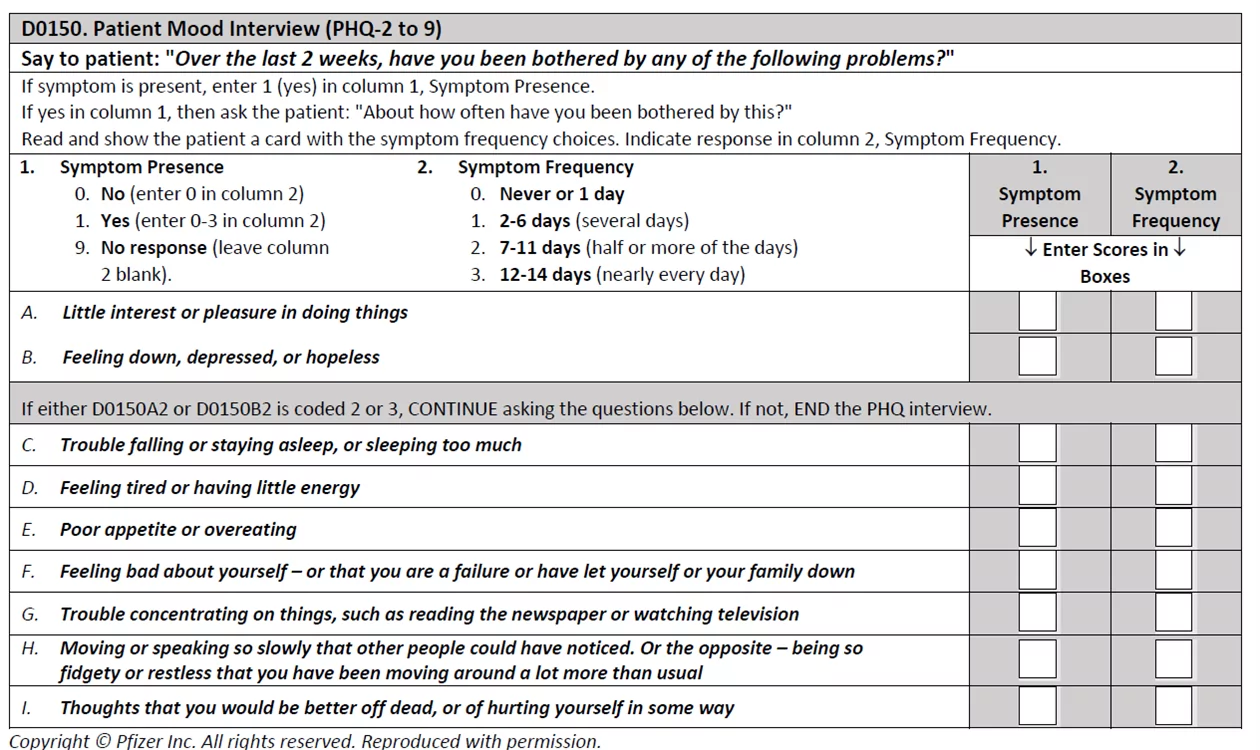
The Patient Health Questionnaire PHQ-2 to 9 is a validated interview that screens for symptoms of depression. It provides a standardized severity score and a rating for evidence of a depressive disorder. This assessment will be completed at SOC, ROC and DC.
The PHQ-2 has been on the last few versions of the OASIS, but on the OASIS – E tool, it is now expanded from the PHQ2 – PHQ9 and assesses mood based on how the PHQ2 is answered.
This item identifies the presence of signs and symptoms of mood distress, a serious condition that is underdiagnosed and undertreated in home health and is associated with significant morbidity. It is particularly important to identify signs and symptoms of mood distress among home health patients because these signs and symptoms can be treatable.
Depression can be associated with:
- Psychological and Physical Distress
- Decreased Participation in Therapy and Activities
- Decreased Functional Status
- Poorer Outcomes.
Interviewing and Coding Tips are available for review in the OASIS – E Guidance Manual. This item identifies the severity score calculated from responses to the PHQ-2 to 9, item D0150. It is important to consider:
- The score does not diagnose a mood disorder or depression but provides a standard score which can be communicated to the patient’s physician, other clinicians, and mental health specialists for appropriate follow up.
- The Total Severity Score is a summary of the frequency scores on the PHQ-2 to 9 that indicates the extent of potential depression symptoms.
Tips for Success
Considerations should be made for additional time needed to complete the OASIS evaluations. Refer to the OASIS – E Guidance Manual for instructions and proposed cue cards to use if necessary. To administer and code the assessment properly, clinicians should understand that it is a structured interview and must be assessed in a specific way. Therefore, education, training, and competency in conducting this assessment is recommended. Reviewing your current policies and procedures and making changes to accommodate the updated OASIS – E assessment is also suggested.
If you would like more information on OASIS-E please reach out to [email protected].
Resources:
1. https://healthrevpartners.com/bims-test-inside-oasis-e/
2. OASIS – E Guidance Manual, Effective 1/1/2023, Centers for Medicare and Medicaid Services
3. https://www.carevoyant.com/home-health-blog/home-health-oasis-e-changes-a-primer
