Author: Alice Shumate, RN
Posted Date: 4/26/22
A final rule has been established for the advent of Home Health Value-Based Purchasing (HHVBP) that fundamentally changes the model of payment for home health services from the simplicity of volume-based to a more complex reimbursement process that utilizes quality and outcomes for calculation.
The decision to officially shift everyone to this new system was based on the results of the original model that was launched by the Centers for Medicare and Medicaid Services (CMS) in 2016 which included 9 participating states representing every geographic area of the continental US (HH PPS final rule 80 FR 68624). The specific focus and purpose were to provide Medicare-certified home health agencies (HHAs) with incentives to provide higher quality and more efficient care and a means to measure and report the results and outcomes. This demonstration resulted in both an average of 4.6 percent improvement in the total performance scores (TPS) for HHAs and an average annual savings of over $140 million for Medicare with no evidence of the presence of adverse risks. Further, there was a reduction in the rate of unplanned acute care hospitalizations and skilled nursing facility (SNF) admissions which in turn provided additional savings on the spending by Medicare in those areas overall.
Expansion of HHVBP
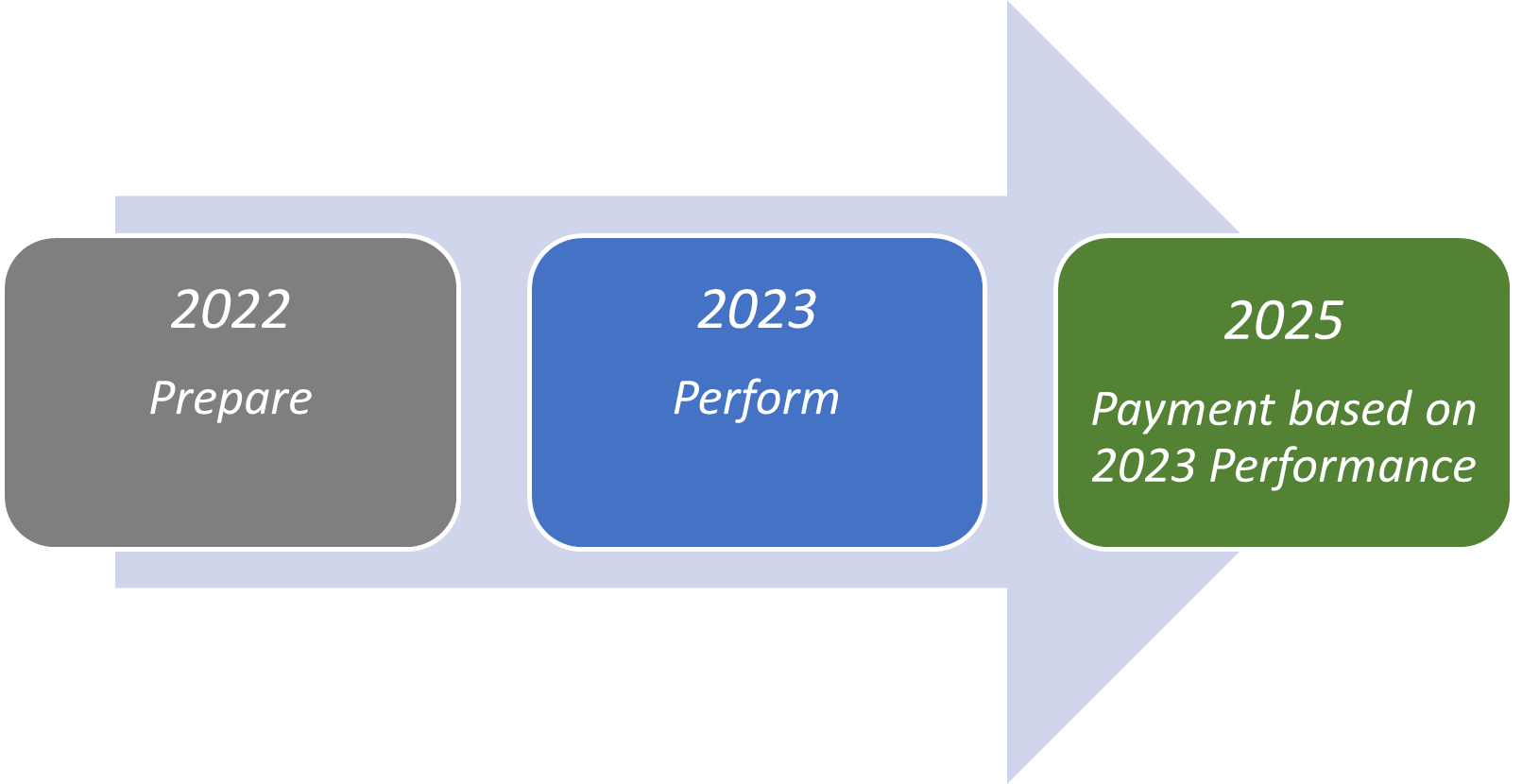
These results were the driving force behind CMS’ decision to expand this model across all 50 states, the District of Columbia, and the U.S. territories. Beginning on January 1, 2022, the pre-implementation year commenced allowing all home health providers the time to implement and exercise this new payment model without payment impact prior to the first full performance year that begins on January 1, 2023. The resulting outcomes experienced in 2023 will determine the final payment with adjustments that will be paid in the calendar year 2025. In other words, what happens next year will be the basis of calculation for the payment each HHA will receive in 2025.
How HHVBP Payment Model Is Calculated
While this shift in the payment model for home health requires additional focus at a time when our industry is already challenged with staff retention, the effects of the pandemic, and other recent CMS mandates like PDGM, there is good news - the data utilized to drive this model will not require additional data collection efforts on your part. All elements involved in this endeavor are already included in existing data generated by each agency. That reduces the learning curve and avoids the impact of integrating a new process which in turn reduces the burden on your operation – that’s good news.
The expanded HHVBP model is predicated on a set of quality measures that are considered relative to your agency’s peers’ performance – a weighted measure approach. Further, CMS has established two cohorts that will consider peer status that is based on each HHA’s beneficiary count in the prior calendar year – one for a larger volume and one for a smaller volume. This helps to create a fairer playing field for comparison of agencies similar in size that considers the effects of volume, available resources, scale, achievement thresholds, etc. for determining adjustments in payment.
This newly expanded HHVBP model will drive payment adjustments on Medicare fee-for-service payments based on elements from the following sources and quality measures:
OASIS-based
- Improvement in Dyspnea / Dyspnea
- Discharged to Community
- Improvement in Management of Oral Medications / Oral Medications
- Total Normalized Composite Change in Self-Care / TNC Self-Care
- Total Normalized Composite Change in Mobility / TNC Mobility
Claims-based:
- Acute Care Hospitalization During the First 60 Days of Home Health Use / ACH
- Emergency Department Use without Hospitalization During the First 60 Days of Home Health / ED Use
HHCAHPS Survey-based:
- Care of Patients / Professional Care
- Communications between Providers and Patients / Communication
- Specific Care Issues / Team Discussion
- Overall rating of home health care / Overall Rating
- Willingness to recommend the agency / Willing to Recommend
More information can be found on the CMS Innovation site related to the overall weighting of TPS and their placement in the HHVBP model.
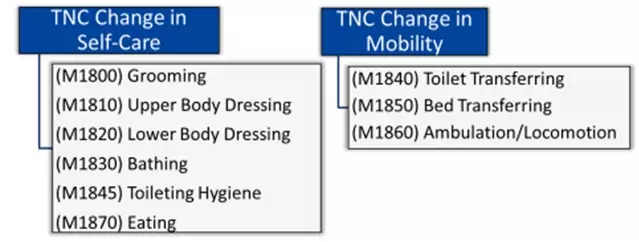
Specific to HHVBP calculations, CMS will utilize composite measures Total Normalized Composite (TNC) Change in Self Care and TNC Change in Mobility to capture the magnitude of change including factors not limited only to improvement:
Exhibit 1. OASIS items included in TNC Measures (Computing the HHVBP Composite Measures (cms.gov))
CMS is using a 5-step process to calculate the two TNC measures above. Steps 1 – 3 pertain to the quality episode and steps 4 – 5 inform the values of the agency level calculation.
Exhibit 2. 5-Step Process for computing the TNC Change in Self-Care and TNC Change in Mobility measures
(Computing the HHVBP Composite Measures (cms.gov))
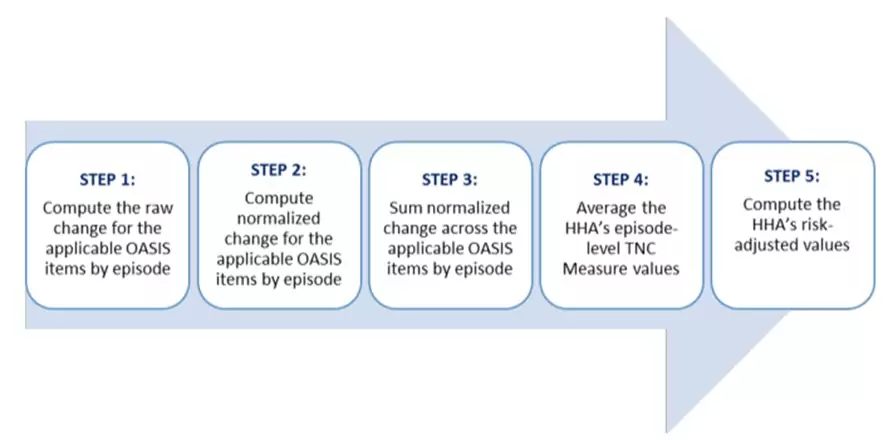
Details can be found on the CMS Innovation site, but below is a high-level breakdown of the 5 steps listed above.
Step 1: For the purposes of calculating each TNC measure, the definition of Quality Episode is as follows: CMS calculates the raw change for each OASIS item (6 for Change in Self-Care and 3 in Change in Mobility above) the difference between the patient’s status as SOC/ROC and the patient’s status at discharge. Should the patient be fully independent at SOC/ROC then that patient will experience either a neutral change or a decline but not an improvement.
Step 2: To compute the Normalized Change for each OASIS item used to compute the TNC measure score, CMS normalizes the quality episode raw change by dividing the value by the maximum possible change for each applicable OASIS item, rendering a range of -1 and +1.
Step 3: Next, the normalized change scores are summed for each quality episode for all the OASIS items used in the TNS Measures above.
Step 4: CMS will average the quality episode level TNC Change in Self-Care or TNC Change in Mobility scores for the patients who have been under care for the agency. The resulting range can span from -6 to +6 for TNC Change in Self-Care and -3 to +3 for TNC Change in Mobility.
Step 5: The TNC Change in Self-Care and TNC Change in Mobility observed scores for the HHA are risk-adjusted based on the standard formula used for all other OASIS measures:
HHARisk-Adjusted = HHAObserved + (NationalPredicted - HHAPredicted)
Detailed examples can be found at Computing the HHVBP Composite Measures (cms.gov) The following table from that site outlines what these steps may look like as a resulted calculation:
Exhibit 3. Status summary for Ms. L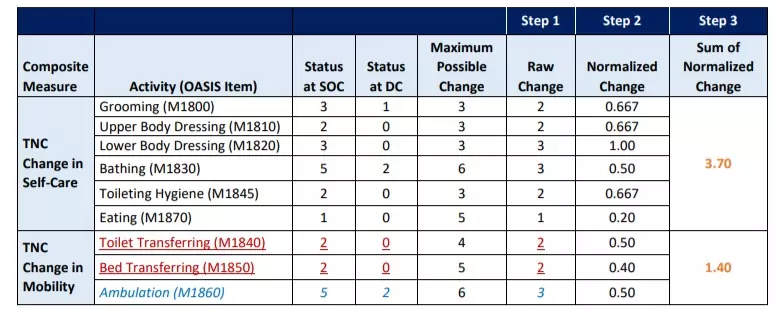
Of note: Measure exclusions for the home health quality episodes are as follows:
- Patient was non-responsive at SOC/ROC as measured by OASIS M1700 / M1710 / M1720
- Home health agencies with less than 20 eligible quality episodes in a given performance period
- Exclusions similar to HHQRP:
- Payment source other than Medicare (traditional fee-for-service), Medicare (HMO / managed care / Advantage Plan), Medicaid (traditional fee-for-service) or Medicaid (HMO/managed care)
- Patient with the following circumstances:
- Less than 18 years of age
- Receiving pre-and/or post-partum maternity services
- Receiving personal care only
Final Thoughts
As stated above, 2022 offers the opportunity for a pulse check on how your agency is performing in these key areas today so you can course-correct and be ready to shine in 2023. Seize the day and celebrate your successes and preparation!
Sources
https://www.federalregister.gov/documents/2015/11/05/2015-27931/medicare-and-medicaid-programs-cy-2016-home-health-prospective-payment-system-rate-update-home
https://www.govinfo.gov/content/pkg/FR-2020-05-08/pdf/2020-09608.pdf
https://innovation.cms.gov/innovation-models/expanded-home-health-value-based-purchasing-model
